Injury Risk and Prevention: Soccer
Soccer (pronounced football to the rest of the world) is one that is very inclusive – age and gender need not matter. If you are a parent, this is one of the first sports you may enroll your child in. The actual gameplay when they are first introduced to the sport may not be the most important aspect, but the skills of fair play, teamwork, and physical activity are the utmost priority of youth soccer programs.
However, as they get older, the competitive component of soccer takes over – speed of play, skill of the players, and the drive to win (be it at a house league or travel team level) will all increase. The consequence of increased gameplay is that the risk of injury undoubtedly increases. Can certain injuries be prevented? If so, how can it be done?
As a health care practitioner, there are a number of “pre-season” screens that can be done to evaluate an individual in a number of measurable: baseline concussion testing (discussed in two articles I wrote for CKSN, Concussions In Sport, and Concussion Return To Play Protocol), pre-season flexibility/movement measures, strength, and motor skills. A number of assessment tools are out there, and there are screens that a sports-focused practitioner will most likely use to evaluate an individual.
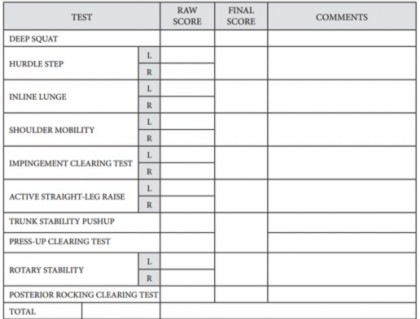
The Functional Movement Screen (FMS)
The FMS is a measure that runs each athlete through 7 movement tests, and 3 clearing tests that they perform to make sure there isn’t any limitations (scoring sheet below). Each movement is assessed on a 3 point scale, and each test will challenge different areas of the body. From this, a guideline as to which exercises might improve these measures can be derived. For example, if an athlete can’t perform an adequate active straight-leg raise, performing core strengthening with hamstring flexibility exercises should improve the measure when re-tested.
The FMS has moderate to good inter-rater and intra-rater reliability, seen in a 2012 study, and it was shown that FMS scores improved following an off-season intervention program put in place with professional soccer players.
The Selected Functional Movement Assessment (SFMA)
If the FMS were in Star Wars, the FMS would be the padawan learner, but the SFMA is the Jedi Master. The Selective Functional Movement Assessment (SFMA) is a clinical assessment system designed to identify musculoskeletal dysfunction by evaluation of fundamental movements for limitations or symptom provocation. The SFMA (seen below) is used in a health care standpoint not to just assess to evaluate movement competency, but to breakdown the movements as to why the individual has a movement issue. If someone can’t perform an overhead squat, is it because of shoulder, hip, knee, or ankle mobility issues? Is it a stability issue? The SFMA breaks that down. Using 10 global movements, a person is measured as competent or not, and the practitioner can go into each pattern to find the true root of the issue. Once again, the SFMA has good intra-rater and inter-rater reliability (Glaws et al., 2014)
Now that we know which assessment tools are out there if you wish to have your athletes tested during the pre-season or at the beginning of the season to address any issues or use it to focus off field training, which injuries are common in soccer?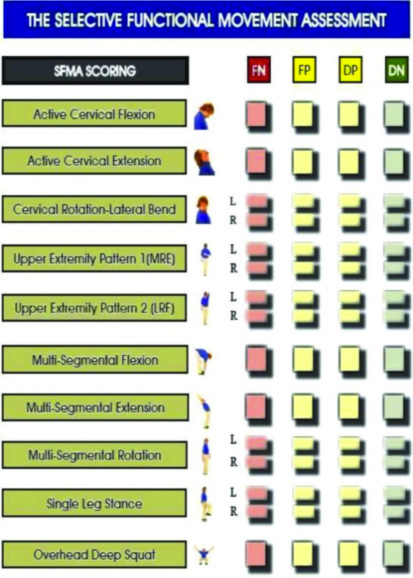
Classification of Soccer Injuries
Injuries happen. As the old phrase goes, “it’s called an accident for a reason”. The five most common causes of sport and recreational injuries across development, in order, were: basketball, football, bicycling, playgrounds, and soccer (Schwebel & Brezuasek, 2014). When examining soccer injuries, the most frequent presented injuries were contusions and sprains of the lower extremity. Between 60 – 90 % of all soccer injuries were classified as traumatic (caused by a collision, soccer ball, etc) and about 10 – 40 % were overuse injuries (Faude et al., 2013). Further breaking down the lower limb injuries, the knee was the most commonly injured body part, with 73.9% of injuries occurring here. The types of injuries were categorized as “less serious” knee dysfunctions (patellofemoral dysfunction or patellar tendon/ligament issues (Barber Foss et al., 2014), but other sprains/strains around the knee can occur. The ankle was the second most commonly injured body part in the lower limb, and accounted for 16.4% of all injuries. Other injuries can occur, but the focus of this article will be on trying to prevent tendon and ligament issues of the lower limb, with particular interest in patellar (kneecap) discomfort, hamstring issues, Achilles tendon issues, and internal knee ligament issues (with focus on the anterior cruciate ligament, or ACL)
Ligament/ Tendon Issues in the Lower limb
A tendon problem is known medically as a tendinopathy, and occurs when the insertion of the muscle to a bone (known as a tendon) get irritated due to repetitive use or gets pulled (known as a strain). A 2015 study in the Journal of Sports Medicine Science (Peters et al.) looked at preventative interventions for tendinopathies and found that to help prevent Achilles tendon issues, having shock absorbing insoles could have a preventative effect. For strategies that are often though of for prevention of tendinopathies, there was no evidence found for stretching exercises, and limited evidence for long-term balance training exercises. The study did note that more research is needed, as there are a number of factors that may contribute to injury.
Another study done by De Vries et al. (2015) looked at using a patellar strap (strap placed just below the kneecap) and its effects on individuals who have patellar tendon pain. The study found that there was a small improvement in proprioception (body awareness), which may lead to a lower risk of patellar tendon issues. Once again, there are a number of factors that may contribute to injury.
Hamstring strains/tendinopathies occur very frequently in soccer, as there is a lot of sprinting involved with the sport. The hamstring muscle group is the collection of the muscles on the back of the thigh. An exercise, known as the Nordic hamstring exercise (pictured below) was introduced in 2001 and has been shown to reduce the risk of acute hamstring injuries in soccer by at least 50%. However, a 2015 study published in the British Journal of Sports Medicine looked at 50 professional teams, with the likes of 32 teams from the UEFA Champions League. The study looked at implementation of this Nordic hamstring program, and found that compliance to the program happened in 16.7% of clubs, with non-compliance in 83.3% of clubs. Recommendations that are not implemented happens in the health world all the time, where it takes a while for doctors to implement the best research available, so it is unfortunately the case with implementing a program like the Nordic. At a youth level, improving coach education that addresses relative advantage, compatibility, and the lack of complexity to implement an injury prevention program must be of high priority (Norcross et al., 2015)
The ACL is one of the 2 internal knee ligaments that if ruptured, takes a long time to recover from. The most common playing situation leading to injury in soccer was pressing forward combined with kicking or heading the ball (Walden et al., 2015). When this happens, the players’ knee falls into what is known as a valgus collapse (see image below), which is one of the mechanisms of injury for the ACL.
Most pediatric athletes presenting to a sports medicine clinic with an ACL injury are between the ages of 13 to 17, with more girls having an increase in ACL injury during puberty (vs. boys). This risk continues to increase as age increases in women, as they become stronger and produce more forceful movements (Hewett et al., 2015). Because of this, ACL prevention strategies are of great importance between the ages of 5 to 12 (Stracciolini et al., 2015).
Another risk factor of ACL injury is the imbalance between the contractions of the quadriceps muscle group (front of the thigh) and the hamstring muscle group (Shultz et al., 2015). One way to potentially train the muscles to work together better is to have athletes perform “Single Leg Drops” (SLDs), starting with a stable surface (like stairs), and progressing to an unstable surface (like a Bosu/stability ball).
Now, there a number of different pre-game exercises, warm-ups, and drills that coaches can use, but which one is the best? How easily can it be implemented?
Trainers – Introducing the FIFA 11+
FIFA, the major soccer organization, teamed up with a number of organizations and companies to create the FIFA 11+. “The 11” is a prevention program for amateur players, consisting of warm-up drills that should be done at least two times a week, and has a modified version on game days. The warm up is 20 minutes in length, and consists of three parts.
Part 1: running exercises at a slow speed combined with active stretching and controlled partner contacts
Part 2: six set of exercises, focusing on core and legs strength, balance, and plyometrics/ agility, each with three levels of increasing difficulty;
Part 3: running exercises at moderate/high speed combined with planting/cutting movements
In Switzerland, there was a nationwide implementation of the program between 2004-2008, and its implementation lead to a 30-50% decrease in injuries (Barengo et al, 2014). It also showed that the athletes had improved neuromuscular and motor performace, which could translate into other sports/movement based activities. Basically, it is awesome, and every trainer/youth coach should implement it.
Is it expensive? Is it hard to implement? No, and no. It is all free, and found here: http://f-marc.com/11plus/home/
With our youth, being able to prevent as many injuries as possible is critical. From pre-season screening, going to see a health care practitioner, and having a solid training plan in place (done by the coach or team trainer), the collective group will be able to minimize the risk of injuries. Not all can be prevented, but if the athlete is doing as much as they can to keep everything flexible and strong, then the risk will be greatly reduced.
References
Schwebel DC1, Brezausek CM. J Athl Train. 2014 Nov-Dec;49(6):780-5. doi: 10.4085/1062-6050-49.3.41. Child development and pediatric sport and recreational injuries by age.
Barber Foss KD1, Myer GD, Hewett TE. Phys Sportsmed. 2014 May;42(2):146-53. doi: 10.3810/psm.2014.05.2066. Epidemiology of basketball, soccer, and volleyball injuries in middle-school female athletes.
Faude O1, Rößler R, Junge A. Sports Med. 2013 Sep;43(9):819-37. doi: 10.1007/s40279-013-0061-x.
Football injuries in children and adolescent players: are there clues for prevention?
de Vries AJ1, van den Akker-Scheek I2, Diercks RL2, Zwerver J2, van der Worp H2. J Sci Med Sport. 2015 May 14. pii: S1440-2440(15)00098-5. doi: 10.1016/j.jsams.2015.04.016. [Epub ahead of print]. The effect of a patellar strap on knee joint proprioception in healthy participants and athletes with patellar tendinopathy
Peters JA1, Zwerver J2, Diercks RL2, Elferink-Gemser MT3, van den Akker-Scheek I4. J Sci Med Sport. 2015 Apr 1. pii: S1440-2440(15)00080-8. doi: 10.1016/j.jsams.2015.03.008. [Epub ahead of print]. Preventive interventions for tendinopathy: A systematic review.
Br J Sports Med. 2015 May 20. pii: bjsports-2015-094826. doi: 10.1136/bjsports-2015-094826. [Epub ahead of print]. Evidence-based hamstring injury prevention is not adopted by the majority of Champions League or Norwegian Premier League football teams: the Nordic Hamstring survey.
Norcross MF1, Johnson ST2, Bovbjerg VE2, Koester MC3, Hoffman MA2. J Sci Med Sport. 2015 Apr 1. pii: S1440-2440(15)00081-X. doi: 10.1016/j.jsams.2015.03.009. [Epub ahead of print]. Factors influencing high school coaches’ adoption of injury prevention programs.
Stracciolini A1, Stein CJ2, Zurakowski D3, Meehan WP 3rd1, Myer GD4, Micheli LJ2. Sports Health. 2015 Mar;7(2):130-6. doi: 10.1177/1941738114554768. Anterior cruciate ligament injuries in pediatric athletes presenting to sports medicine clinic: a comparison of males and females through growth and development.
Shultz R1, Silder A2, Malone M3, Braun HJ4, Dragoo JL1. Sports Health. 2015 Mar;7(2):166-71. doi: 10.1177/1941738114565088. Unstable Surface Improves Quadriceps:Hamstring Co-contraction for Anterior Cruciate Ligament InjuryPrevention Strategies.
Waldén M1, Krosshaug T2, Bjørneboe J2, Andersen TE2, Faul O2, Hägglund M3. Br J Sports Med. 2015 Apr 23. pii: bjsports-2014-094573. doi: 10.1136/bjsports-2014-094573. [Epub ahead of print]. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases.
Hewett TE1, Myer GD, Kiefer AW, Ford KR. Med Sci Sports Exerc. 2015 May 12. [Epub ahead of print]. Longitudinal Increases in Knee Abduction Moments in Females during Adolescent Growth.
Teyhen DS, Shaffer SW, Lorenson CL, Halfpap JP, Donofry DF, Walker MJ, Dugan JL, Childs JD. J Orthop Sports Phys Ther. 2012 Jun;42(6):530-40. doi: 10.2519/jospt.2012.3838. Epub 2012 May 14. The Functional Movement Screen: a reliability study.
Kiesel K1, Plisky P, Butler R. Scand J Med Sci Sports. 2011 Apr;21(2):287-92. doi: 10.1111/j.1600-0838.2009.01038.x. Functional movement test scores improve following a standardized off-season intervention program in professional football players.
Glaws KR, Juneau CM, Becker LC, Di Stasi SL, Hewett TE. Int J Sports Phys Ther. 2014 Apr;9(2):195-207. Intra- and inter-rater reliability of the selective functional movement assessment (sfma).
Barengo NC1, Meneses-Echávez JF2, Ramírez-Vélez R2, Cohen DD3, Tovar G4, Bautista JE5.
Int J Environ Res Public Health. 2014 Nov 19;11(11):11986-2000. doi: 10.3390/ijerph111111986. The impact of the FIFA 11+ training program on injury prevention in football players: a systematic review.